A Hysterectomy is a gynecological procedure that usually entails removing the entire uterus, including the cervix. There are different types of hysterectomies: Supracervical Hysterectomy, which entails removing the uterus while leaving the cervix in place, and Total Hysterectomy, which entails removing the uterus along with the cervix.
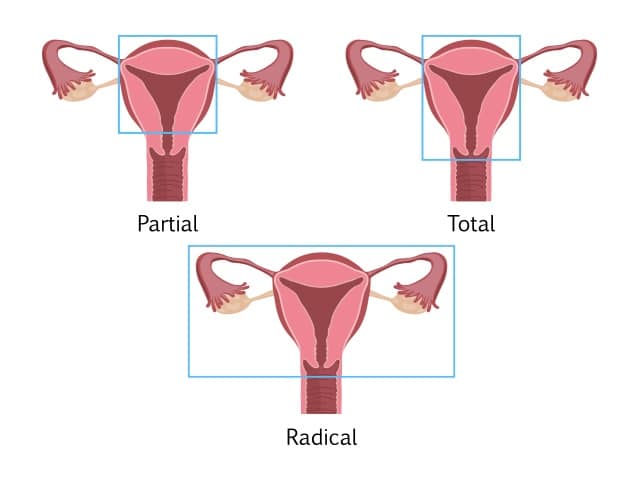
The term Hysterectomy, whether total or supracervical, is only specific to surgery on the uterus and does not include removal of the ovaries.
Removing the ovaries along with the uterus is not recommended in patients under 65 years old, unless indicated by your doctor. Removing the ovaries with a Hysterectomy is referred to as Oopherectomy.
It is recommended at the time of Hysterectomy to remove the fallopian tubes as well. Studies have shown that removing the fallopian tubes during a Hysterectomy can decrease the risk of future cancer of the ovaries and fallopian tubes by 30%.
Hysterectomies are performed to relieve the following conditions:
- Adenomyosis
- As part of pelvic prolapse repair
- Heavy bleeding, with or without Fibroids
- Pelvic pain with origin in the uterus
- Painful intercourse with origin in the uterus
At CEAPS, our preferred method of performing Hysterectomies is through a minimally invasive approach that could be done successfully in almost all cases, irrelevant of the size of the uterus or the complexity of the procedure.
This technique carries lower risks of complications and requires only small incisions, resulting in quicker recovery.
This procedure is ideal as it gives full access to the pelvis, allowing the doctor to evaluate and treat potential associated conditions, such endometriosis, scar tissue, and ovarian cysts.
After a Hysterectomy, people can be discharged the same day, and be back to their full, normal activity in around 2 weeks typically (aside from sex).
Sexual intercourse should only be resumed after at least 8 weeks, and only if you are feeling comfortable.
You might experience the following after a Hysterectomy:
- General pain that should resolve with time
- Pain around the incisions that should last only a few days
- Pelvic and rectal pain and pressure that should resolve with time
- Chest and shoulder pain that should resolve 2 to 3 days
- Bruises at the incisions that will resolve on their own
- Vaginal spotting during the first week
- Nausea caused by anesthesia and pain medication
- Swelling of the abdomen that will resolve over time
- Constipation due to medication
- Diarrhea caused by antibiotics
- Urinary retention due to anesthetics (seek your doctor’s advice if this occurs after you are sent home)
As part of your recovery, you might be given prescription medication to ease pain. It is important not to drive when taking any prescribed narcotics. Avoid lifting, swimming, and heavy exercise, and use caution when starting an exercise routine after your procedure, starting slowly and listening to your body to make sure you are comfortable and able.
A Hysterectomy will cause periods to stop, however hormone production should not be affected if ovaries are spared during the surgery. After a hysterectomy you are not able to conceive, so this procedure is not recommended for people desiring fertility or childbearing.
A Hysterectomy will not cause early menopause unless both of the ovaries have been removed during the procedure. In this case, Estrogen replacement therapy can be used to prevent menopausal symptoms, such as hot flashes, vaginal dryness, and night sweats. You can discuss this with your doctor, based on the procedure you undergo and what is best for your body.
Dr. Moawad has had a high success rate of minimally invasive surgeries over the past 10 years, and his work is all about exhausting every option before turning to open surgery as a last resort. With international and national distinction and published work in the field of minimally invasive surgery, along with his work with patients in advocacy groups, Dr. Moawad puts the patient’s wellbeing and recovery above all else.
At CEAPS, we work in the same spirit, performing successful minimally invasive procedures that make the patient’s life easier by shortening recovery time and improving outcomes.