Conditions
At CEAPS, we diagnose and treat various complex gynecological conditions. We believe in taking a patient-centered approach, focusing on the patient’s experience to provide different options with optimal treatment plans for their specific condition. Dr. Moawad advocates for patients to help them understand their conditions and empower them to make informed decisions.
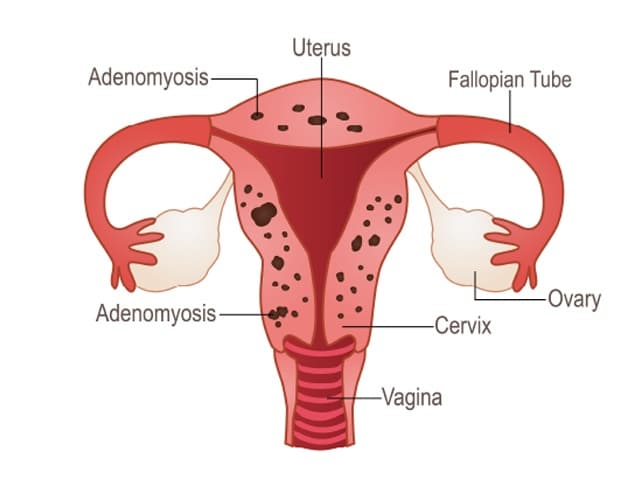
Adenomyosis is defined as ‘the presence of endometrial glands and stroma found within the muscle of the uterus or myometrium. During monthly menstruation, this embedded tissue bleeds and can lead to intense pelvic pain, inflammation and swelling, and heavy bleeding.
This condition is oftentimes misunderstood or even misdiagnosed, as Adenomyosis, often referred to as Endometriosis of the muscle of uterus, causes both painful and heavy periods, painful sex, or dyspareunia.
With Endometriosis, spots of endometrial lining are located outside of the uterus, while in the case of Adenomyosis, this tissue is inside the muscle of the uterus… or an “Inside-Out Endometriosis”, as it used to be known.
To date, there are no clear causes of Adenomyosis, which can be frustrating. Studies have shown that people who have given multiple births and who already suffer from Endometriosis are more at risk for Adenomyosis.
To diagnose Adenomyosis, a doctor will examine you and assess your symptoms. With this condition, the uterus may feel big, soft, tender, and very sensitive to the touch.
Tests that can be performed by your doctor are:
- Ultrasound
- MRI
- Pathology examination after a Hysterectomy procedure
As far as treatment goes, the symptoms of Adenomyosis can be dealt with by taking pain medication or by preventing monthly menstruation with hormonal treatment:
- Pain medication: The pain associated with Adenomyosis can be debilitating. Analgesics, anti-inflammatories, or strong painkillers can be prescribed.
- Hormonal Treatment: This is not a cure, as the pain will return if the treatment is stopped. Oral contraceptive pills and contraceptive implants (hormonal IUD), or injections can be suggested by your doctor to relieve pain and stop monthly periods.
- Surgery: If Adenomyosis is localized, it could be surgically excised. Sometimes the only solution to Adenomyosis is to remove the entire uterus. This procedure is called a Hysterectomy and may be suggested by your doctor based on your medical history, extent of pain, and other symptoms.
Cervical Insufficiency, also known as Cervical Incompetence is the inability of the uterine cervix to retain a pregnancy in the absence of contractions in the second trimester. With this condition, the cervix begins to dilate and thin before the pregnancy has reached term. Cervical insufficiency can occur in a single pregnancy, or may be recurrent.
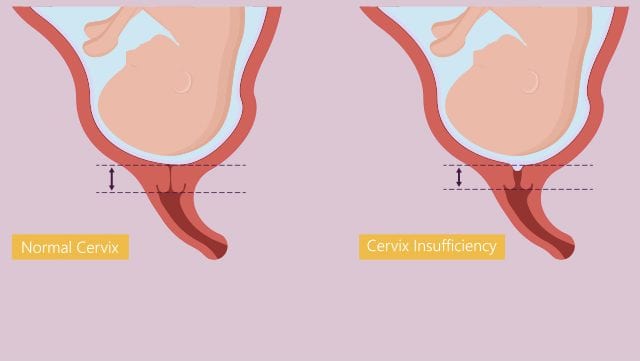
It has profound implications for both maternal and neonatal outcomes, including losing a pregnancy, premature delivery and prolonged bed rest during pregnancy.
Cervical Insufficiency can be caused by one or more different factors, including:
- Previous surgery performed on the cervix
- Damage to cervix during a previous difficult child birth
- Birth defect resulting in a malformed cervix or uterus
- Trauma to the cervix from procedure to terminate a miscarriage
- Exposure to DES (Diethylstilbestrol)
If you have had a miscarriage after your second or third trimester, your doctor may check for Cervical Insufficiency. You may also undergo an ultrasound before pregnancy or early on in your pregnancy if you have any potential risk factors for this condition.
Your doctor will examine you through:
- Ultrasound
- Pelvic exam
The treatment for a Cervical Insufficiency is a procedure to close and reinforce the opening in the cervix. This is performed between 14-16 weeks of the pregnancy, or could be done before the pregnancy. This procedure is called a Cervical Cerclage and is performed primarily through vaginal route. In case of failure of the cerclage or inability to perform through the vaginal route, an abdominal approach is then preferred. This procedure is called a Transabdominal Cerclage, also known as a TAC.
At CEAPS, Dr Moawad’s extensive research on the subject, and his advanced training in performing these procedures, enables patients to have a successful, less morbid minimally invasive procedure with a high success rate.
Fibroids are non-cancerous growths consisting of muscle and fibrous tissue located inside the uterus and varying in size. Some Fibroids are just a few inches big, and others may take up the whole abdominal cavity.
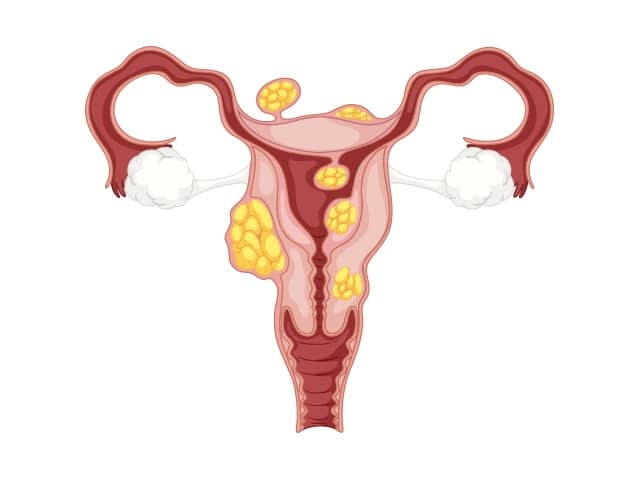
Fibroids are quite common in people of reproductive age, affecting 85% of women. Most Fibroids usually go undetected and cause no symptoms, though Fibroids can cause a variety of symptoms including abnormal vaginal bleeding, abdominal and pelvic pain ….
Fibroids are named depending on their location:
- Subserous Fibroids: Grow in the muscle of uterus, expanding outside the uterus into the pelvic area
- Intramural Fibroids: Grow within the muscle of the uterus
- Submucosal Fibroids: Grow towards the inner wall and expand in the the endometrial cavity
Generally speaking, Fibroids, no matter their type, grow slowly. However, among many factors, high levels of Estrogen can make these Fibroids grow faster.
Typically, Fibroids are benign tumors. They could, although rarely become cancerous, with this only happening in between 1 in 500 and 1 in 2000 people.
As mentioned, most people with Uterine Fibroids experience no symptoms. However, 1 in 3 people with Fibroids experience symptoms, mostly related to the size and the location of the Fibroids.
These symptoms include:
- Heavy bleeding during periods with blood clots and cramps
- Abdominal or lower back pain
- Frequent need to urinate
- Constipation
- Deep pain during sex
- Infertility or difficulty conceiving
Any person of reproductive age can get Fibroids, from puberty on to menopause. Because their growth is related to the hormone Estrogen, Fibroids can potentially shrink away after the onset of Menopause.
To diagnose Fibroids, your doctor will ask for a medical history and a pelvic exam. Large Fibroids can be detected through vaginal or abdominal examinations.
Tests to detect Fibroids may include:
- Blood tests to detect anemia associated with heavy periods, a symptom of Fibroids
- Utrasound
- MRI
Treating your Fibroids will depend on the symptoms associated with this condition. It also depends on their size, location, and your future plans for fertility.
Most of the time, Fibroids can be left untouched and just monitored. You may be prescribed medication to treat symptoms of pain or heavy periods. Other times, Fibroids might need to be surgically removed. This is a shared decision that you can make with your doctor based on your evaluation.

AUB, Abnormal Uterine Bleeding, or sometimes referred to as Abnormal Vaginal Bleeding, is a term used to refer to heavy periods or bleeding in between normal periods. It is a common condition affecting around 10% to 20% of women in the US.
Menorrhagia, also known as heavy periods, occurs when there is loss of excessive blood during monthly menstrual cycles.
Metrorrhagia, also known as bleeding between periods, occurs when there is bleeding from the uterus between menstruations.
AUB is not just uncomfortable and inconvenient, but it can also affect the person’s quality of life whether physical, mental, or emotional.
This condition is not always associated with physical abnormalities. Approximately 40% to 60% of people with heavy periods have no specific underlying cause.
AUB is associated with:
- Leaking through sanitary pads
- Necessity for double protection
- Flooding of menstrual blood onto clothes
- Large clots in blood
- Sensations of weakness, tiredness
- Anemia
- Planning daily life around menstruation
Although the majority of people with AUB have no specific underlying cause, there are some known reasons :
- Polyps: non-cancerous growths in lining of the uterus
- Endometriosis: when developed in the vagina and/or the lower uterus
- Fibroids: benign growths on the walls of the uterus
- Adenomyosis: when glands from uterus lining embed in the muscle of the uterus
- Cancer: uterine cancer is uncommon but can cause heavy periods
- Thyroid disease: thyroid disease can cause tiredness, weight gain, changes in hair and skin, intolerance to cold, and AUB
- Clotting problems: platelet problems or certain diseases can affect clotting and increase AUB
- Medical treatments: some medical treatments such as hormonal contraceptives, anticoagulants, and anti-cancer drugs can cause AUB
Rather than just identifying AUB, your doctor will probably want to investigate the causes.
Your doctor can ask for some tests, which include:
- Blood tests
- Ultrasound
- Hysteroscopy (a camera to visualize the cavity of the uterus)
As for treatments, there are many options available, including:
- Hormonal and non-hormonal treatments
- Endometrial ablation
- Minimally invasive surgical removal of fibroids and polyps
- Hysterectomy
Ovarian Cysts are growths developing within the ovaries. Most Ovarian Cysts are harmless and are not cancerous. Cysts on the ovaries can sometimes grow as big as a watermelon, where a normal ovary is around the size of an almond.
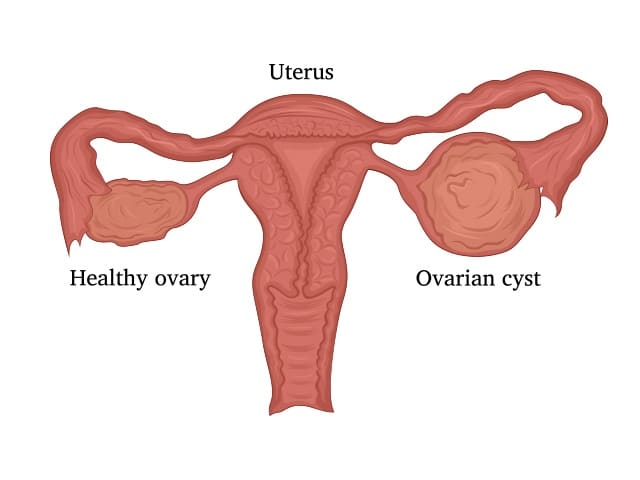
Ovarian Cysts are most common before Menopause, occurring in around 7% of women.
Although Ovarian Cysts are not necessarily harmful or cancerous, they should be taken seriously, because they could indicate other underlying conditions. Identifying and examining Ovarian Cysts is necessary to rule out cancer and any underlying causes, such as Endometriosis.
Ovarian Cysts can come in many different forms, each with a different cause:
- Functional cyst: These cysts form because of normal function of the ovaries. When ovulation does not happen and a follicular cyst remains in the ovaries, and the opening where the egg escapes is closed off with accumulated fluid.
- Pathological cyst: These cysts form because of disease, but are not necessarily cancerous.
- Dermoid cysts: These cysts grow with the existence of developmental tissue that can contain teeth, bone, or hair.
- Hemorrhagic cysts: These cysts form due to bleeding.
- Endometriomas: These cysts are caused by Endometriosis, and are a sign of a severe form of the condition, accompanied with a lot of pain.
- Cancerous cysts: These cysts are rare, but commonly affect post-menopausal people, with vague symptoms that can go undiagnosed.
With Ovarian Cysts, most symptoms are not always noticeable. With Endometriomas however, the main symptom is severe pain, even when the cysts are small in size.
If the cysts are large, regardless of their type, symptoms can include pain and swelling in the abdominal area. Cysts can also lead to constipation or frequent urination due to the cysts pressing on other organs in the abdomen.
Complications of Ovarian Cysts can include twisting of the ovary, bleeding, or bursting of cysts, which can cause severe pain and bleeding, usually requiring emergency attention and treatment.
Diagnosing Ovarian Cysts can be done through assessing medical history and by examination. These tests include:
- Ultrasound
- Blood tests
- MRI
- CT scan
Some cysts should be monitored by your doctor, while others don’t need monitoring at all. Functional Cysts may go away on their own, without being treated.
Some cysts require surgery, and this should be determined by your doctor, depending on the size, appearance, test results, and symptoms.

Painful sex, also known as dyspareunia, is an issue that affects around 10% to 20% of women in the US. This condition may leave some people feeling embarrassed, upset, or ashamed.
While it is normal to have anxieties over such an intimate part of your life, in most cases, Painful sex can be solved through treatment.
With both physical and emotional factors at play, Painful sex issues should be identified and assessed by a specialist, so that you can get the help you need and resume comfortable and pleasurable intimacy.
With Painful sex, it is important to be able to locate and describe the pain you are facing. Different types of pain can be associated with different underlying issues. Assess whether the pain is superficial or deep, if pain during sex is a new occurrence, if inserting a tampon hurts, and how the pain feels in general.
Once you have identified the pain, seek your doctor’s help to pinpoint the causes and potential treatments and solutions.
Painful sex can be caused by various factors, both physical and emotional.
Superficial Dyspareunia, also known as Pain on penetration is pain experienced upon vaginal entry and can be caused by:
- Too little lubrication from menopause and thinning of the walls of the vagina
- Injury, infection, irritation
- Vaginismus: spasms of the muscles of the vaginal wall, making penetration extremely painful
- Vestibulitis: inflammation of the tissues surrounding the entrance to the vagina which can cause intense pain, stinging, and soreness when pressure is applied
- Birth abnormalities
Deep Dyspareunia, also known as deep pain is experienced after initial penetration. It can feel worse upon thrusting or in certain sexual positions, and can be caused by:
- Endometriosis: when developed behind the vagina or the lower uterus
- Pelvic Inflammatory Disease: caused by sexually transmitted infections
- Fibroids: benign growths on the walls of the uterus
- Adhesions: when organs in the pelvic area are scarred and stuck together
- Prolapse: when the uterus drops into the vagina due to pelvic floor weakness
To identify and asses your condition, the doctor will ask for details and information on your experience with painful sex, including history, occurrences, and type of pain. Your doctor may also perform a pelvic examination and order tests such as labs and an ultrasound.
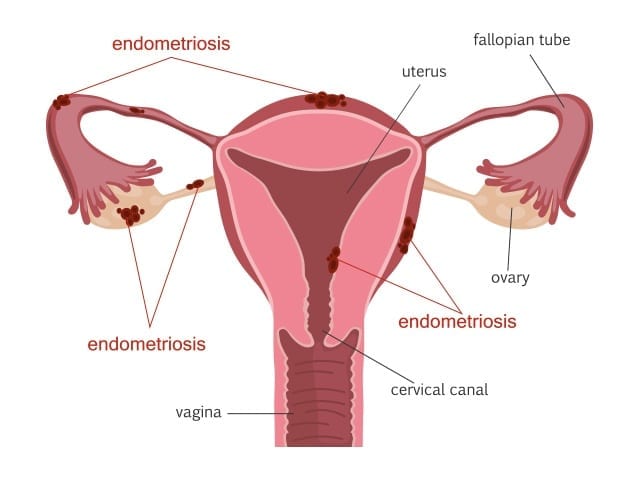
Endometriosis a condition defined by the presence of endometrial-like tissue outside the uterus.
Endometriosis affects the lining of the pelvis (peritoneum), the fallopian tubes, the ovaries and the uterus. It could also affect other pelvic structures like the bladder, the bowels and the pelvic nerves, and could grow outside the pelvis, affecting the lungs, diaphragm, etc.…
1 in every 10 women is affected with Endometriosis during their reproductive years. Although it is a common condition, it is sometimes misdiagnosed or mistreated, taking up to 7 years from the onset of pain to diagnosis.
There are multiple risk factors for Endometriosis that have been identified, however this information must be treated carefully and with caution, as knowledge about the causes and development of Endometriosis is not yet definite. Research is still ongoing to determine what the causes may be.
These risk factors may include:
- Family history of Endometriosis
- Never having given birth
- Short periods
- Heavy and long periods
- Low BMI
- History of high estrogen production
- Late menopause
- Early onset of period
- Reproductive system irregularities
Although sometimes people with Endometriosis can be asymptomatic, many people do experience painful and uncomfortable symptoms, such as:
- Painful periods
- Pelvic pain throughout the cycle
- Intestinal pain
- Fatigue and unease
- Painful sex
- Difficulty conceiving and infertility
- Painful urination or bowel movements
- Blood in urine or bowel near the time of menstruation
- Pain radiating into back, down legs, and sometimes into chest
- Shoulder and neck pain
- Fatigue
- Dizziness with cycle
- Recurring constipation/diarrhea
To identify and diagnose Endometriosis, we can perform the following examinations:
- Pelvic examination
- Ultrasound
- MRI
- Laparoscopy
Endometriosis can be classified in stages:
- Stage One: Minimal Endometriosis
Characterized by minimal superficial lesions and no significant adhesions
- Stage Two: Mild Endometriosis
Characterized by superficial and deep lesions with no significant adhesions
- Stage Three: Moderate Endometriosis
Characterized by multiple deep lesions, small cysts on ovaries, and translucent adhesions
- Stage Four: Severe Endometriosis
Characterized by severe and multiple deep lesions, large cysts on ovaries, and dark adhesions
These stages are based on the location, adhesions, spread, and depth of the Endometriosis and will be determined by your doctor upon examination.
If you have been diagnosed with Endometriosis, there are different treatment options, depending on the stage, symptoms and condition. For some people this disease is manageable, while for others, it is debilitating and causes disruption of daily life and routines.
Treatment can include painkillers for mild conditions, or a minimally invasive surgical excision of Endometriosis.
Endometriosis excision is when the endometriotic lesions are removed surgically while preserving the uterus, fallopian tubes, and ovaries. This type of minimally invasive surgery is the most effective treatment for Endometriosis, and should only be done by trained specialists.
People with severe deep infiltrating Endometriosis benefit highly from excision surgery. The improvement after this procedure for people with such cases is usually striking and highly successful.
Other treatments for Endometriosis include:
- Pelvic floor physiotherapy
- Pelvic floor Botox
- Change in diet
- Acupuncture
- Assessing and avoiding environmental triggers
Cervical Insufficiency, also known as Cervical Incompetence is the inability of the uterine cervix to retain a pregnancy in the absence of contractions in the second trimester. With this condition, the cervix begins to dilate and thin before the pregnancy has reached term. Cervical insufficiency can occur in a single pregnancy, or may be recurrent.
It has profound implications for both maternal and neonatal outcomes, including losing a pregnancy, premature delivery and prolonged bed rest during pregnancy.
Cervical Insufficiency can be caused by one or more different factors, including:
- Previous surgery performed on the cervix
- Damage to cervix during a previous difficult child birth
- Birth defect resulting in a malformed cervix or uterus
- Trauma to the cervix from procedure to terminate a miscarriage
- Exposure to DES (Diethylstilbestrol)
If you have had a miscarriage after your second or third trimester, your doctor may check for Cervical Insufficiency. You may also undergo an ultrasound before pregnancy or early on in your pregnancy if you have any potential risk factors for this condition.
Your doctor will examine you through:
- Ultrasound
- Pelvic exam
The treatment for a Cervical Insufficiency is a procedure to close and reinforce the opening in the cervix. This is performed between 14-16 weeks of the pregnancy, or could be done before the pregnancy. This procedure is called a Cervical Cerclage and is performed primarily through vaginal route. In case of failure of the cerclage or inability to perform through the vaginal route, an abdominal approach is then preferred. This procedure is called a Transabdominal Cerclage, also known as a TAC.
At CEAPS, Dr Moawad’s extensive research on the subject, and his advanced training in performing these procedures, enables patients to have a successful, less morbid minimally invasive procedure with a high success rate.
 Endometriosis can involve almost any organ in the body such as lungs, colon, muscles, eyes, brain, and nerves etc… It is difficult to determine the exact prevalence of extra pelvic endometriosis due to the lack of epidemiological studies and underdiagnosis of this condition.
Endometriosis can involve almost any organ in the body such as lungs, colon, muscles, eyes, brain, and nerves etc… It is difficult to determine the exact prevalence of extra pelvic endometriosis due to the lack of epidemiological studies and underdiagnosis of this condition.
The lining of the uterus that sheds monthly is called the endometrial lining. Genetic and epigenetic factors contribute to the development of lesions that are similar to endometrial tissue in different areas in the body, mainly the pelvis. This results in endometrial-like lesions in different organs which get inflamed and can bleed due to the formation of new blood vessels. These lesions can further undergo fibrosis and scarring and compress nearby structures to cause symptoms accordingly.
When the endometrial-like lesions implant near or along a nerve, they can cause pain and numbness in the areas supplied by this nerve. The sciatic nerve runs from the lower back along the posterior leg downwards. Pain felt along this nerve is termed sciatica and can be due to compression or inflammation of the nerve.
Endometriosis involving the sciatic nerve is very rare but presents with specific, regional symptoms of low back pain, numbness and cramping that extend down the leg.
Signs and Symptoms:
If you have sciatic endometriosis, you will most likely experience pain, numbness, cramping and possibly weakness of your lower back and/or along the back of your leg.
When it’s severe enough, your muscle weakness can prevent you from lifting the front of your foot.
Symptoms can occur any time during the month and might last for several days in intermittent episodes.
If you’re experiencing sciatica that occurs frequently with no obvious reason, it might be worth it to suspect a diagnosis of sciatic nerve endometriosis.
There is almost always history of pelvic endometriosis that accompanies sciatic nerve endometriosis so also look out for symptoms such as pelvic pain, heavy periods, painful intercourse and painful defecation.
Diagnosis:
Like pelvic endometriosis, imaging may aid in the diagnosis of sciatic nerve endometriosis but definitive diagnosis requires surgical visualization of the lesions.
If your doctor suspects sciatic nerve endometriosis, they will order an MRI for you which may show lesions around the sciatic nerve or compression of the nerve but may not always be diagnostic.
In that case, laparoscopic exploration of the nerve area by an expert is advisable for confirmation of the diagnosis.
Treatment:
Treatment is similar to that of pelvic endometriosis in terms of hormonal medications and pain killers for symptom control but laparoscopic surgical excision of the lesions by a well-trained surgeon is preferred to treat the condition.
At CEAPS, we always opt for minimally invasive approaches to provide the best experience for our patients with the least amount of side effects and complications. Sciatic Nerve decompression and excision of sciatic endometriosis is technically challenging and requires A high level of training and expertise.
Choose your surgeon with the training and the experience to manage these complex conditions.
Dr. Moawad is a highly reputable leading expert in this domain.
 Bladder endometriosis is the presence of endometrial-like tissue inside or on the surface of the bladder. It is usually a complication of deeply infiltrating pelvic endometriosis but may rarely develop on its own.
Bladder endometriosis is the presence of endometrial-like tissue inside or on the surface of the bladder. It is usually a complication of deeply infiltrating pelvic endometriosis but may rarely develop on its own.
Urinary tract endometriosis occurs in around 1-5% of patients with endometriosis but this number increases to 19-53% in those with deep infiltrating endometriosis. Bladder involvement comprises around 70-85% of urinary tract endometriosis cases.
Symptoms:
- Frequent or urgent need to urinate
- Pain or burning during urination
- Pelvic pain especially when your bladder is full
- Lower back pain
- Blood in urine
Diagnosis:
If you’re experiencing the any or all of the above symptoms, your gynecologist might need to work you up for bladder endometriosis.
You will first get a pelvic exam and a pelvic ultrasound.
Your doctor may then ask for further imaging such as a pelvic CT or MRI.
A diagnosis can be made by visualizing the lesions with a scope inserted through your urethra into the bladder, a procedure termed cystoscopy, or by laparoscopic visualization of endometriosis involving the bladder.
Treatment:
To treat bladder endometriosis, surgical excision of the lesions is the optimal treatment to improve the symptoms.
Medical treatments are usually symptomatic treatments and will not eradicate or cure the lesions. Medical therapies include hormones such as combined oral contraceptives, gonadotropin releasing hormone agonists or aromatase inhibitors.
Surgery is the optimal management for bladder endometriosis, in which your doctor will remove all the endometriosis tissue growing around the bladder which will relief your symptoms. Surgery may be a combination of laparoscopy and cystoscopy, and could include shaving of the lesions from the bladder or excising part of the bladder ( partial cystectomy).
A transurethral resection (via cystoscopy) is minimally invasive and has a fast recovery time but may lead to incomplete lesion removal and persistence of symptoms. It is not strongly supported by evidence for treatment of bladder endometriosis.
A partial cystectomy, if done by a minimally invasive approach such as laparoscopy or robot, would also provide fast recovery. This procedure provides complete removal of the lesions and allows for treatment of other concomitant pelvic endometriosis. A partial cystectomy also has lower chances of recurrence, providing longer term relief.
At CEAPS, we always opt for minimally invasive approaches to provide the best experience for our patients with the least amount of side effects and complications. Bladder endometriosis excision surgery is technically challenging and requires sometimes a multidisciplinary approach with a urologist.
Choose your surgeon with the training and the experience to manage these complex conditions.
Dr. Moawad is a highly reputable leading expert in this domain.
 Ureter endometriosis is a type of urinary tract endometriosis that involves the ureters. Ureters are the tubes that connect the kidneys to the bladder. When endometrial-like tissue is found on these tubes, we call it ureteral endometriosis. This usually occurs in association with deep infiltrating endometriosis and isolated disease is very rare.
Ureter endometriosis is a type of urinary tract endometriosis that involves the ureters. Ureters are the tubes that connect the kidneys to the bladder. When endometrial-like tissue is found on these tubes, we call it ureteral endometriosis. This usually occurs in association with deep infiltrating endometriosis and isolated disease is very rare.
Involvement of the ureters is relatively rare, comprising 9-23% of all urinary tract endometriosis which themselves are found in only 1-5% of patients with endometriosis.
Most commonly, ureteral endometriosis involves only one ureter with a predominance of the left one but bilateral disease can also occur. Endometriotic lesions may occur anywhere along the ureter and this can lead to different signs, symptoms and complications.
What you may experience if you suffer from ureteral endometriosis:
- 50% of patients remain asymptomatic
- Pelvic pain
- Recurrent urinary tract infections
- Pain during urination
- Renal colic or flank pain
- Blood in urine
The endometriosis nodules may lead to obstruction of the ureter causing backflow of urine into the kidney which results in enlargement of the kidney and possible renal failure.
How will your doctor diagnose ureteral endometriosis?
Your gynecologist will begin with a pelvic exam and an ultrasound.
Further imaging with MRI or CT might be indicated.
Your doctor may also get specific kidney imaging to assess kidney function and size.
Finally, a ureteroscopy would aid in diagnosis as it allows visualization of the nodules and performance of a biopsy for definite diagnosis.
Management:
Treatment of ureter endometriosis is mainly surgical.
Surgical treatment aims to relief ureteral obstruction and avoid recurrence. There is no clearly defined surgical approach and the type of procedure depends on the extent of disease and kidney function. The surgery removes the endometrial-like lesions along with the part of the ureter and possibly reconnect the ureter to the bladder ( ureteral reimplantation) or the ureter to its distal healthy part after removing the damaged portion ( uretero-ureteral anastomosis).
At CEAPS, we always opt for minimally invasive approaches to provide the best experience for our patients with the least amount of side effects and complications. Ureteral surgery is technically challenging and requires sometimes a multidisciplinary approach with a urologist.
Choose your surgeon with the training and the experience to manage these complex conditions.
Dr. Moawad is a highly reputable leading expert in this domain.
 Diaphragmatic endometriosis is another form of extra pelvic endometriosis in which tissue that resembles the endometrial lining grows on the diaphragm. The diaphragm is a muscle that separates the chest from the abdomen and allows us to breathe. It is estimated that around 12% of patients with endometriosis have extra pelvic disease but the prevalence of diaphragmatic endometriosis is unknown.
Diaphragmatic endometriosis is another form of extra pelvic endometriosis in which tissue that resembles the endometrial lining grows on the diaphragm. The diaphragm is a muscle that separates the chest from the abdomen and allows us to breathe. It is estimated that around 12% of patients with endometriosis have extra pelvic disease but the prevalence of diaphragmatic endometriosis is unknown.
If you have diaphragmatic endometriosis, you may be asymptomatic, but you may also experience the following symptoms:
- Chest pain
- Upper quadrant abdominal pain
- Cyclical Shoulder pain
- Pain on breathing
- Cyclical Shortness of breath
Diaphragmatic endometriosis can also present with a combination of symptoms termed Thoracic Endometriosis Syndrome (TES). These include pneumothorax (air in the thorax outside of the lungs), hemothorax (blood in the thoracic cavity), coughing blood or having endometriotic nodules within the thorax.
Diagnosis:
After collecting information on your symptoms, your doctor will examine both your pelvic and abdominal areas. They will order further imaging such as a pelvic and abdominal MRI.
Definitive diagnosis then happens through surgery. Laparoscopic visualization of the endometriotic lesions provides a diagnosis of diaphragmatic endometriosis.
Treatment:
Like pelvic endometriosis, medications may play a role in symptom control but surgical excision of the endometriotic lesions remains the optimal treatment.
Surgery used to be done through a big abdominal incision but laparoscopy and robotic-assisted approaches have been taking over and allow for a minimally invasive approach with quicker recovery and smaller incisions. Ask your doctor about the best surgery for you.
At CEAPS, we always opt for minimally invasive approaches to provide the best experience for our patients with the least amount of side effects and complications. Diaphragmatic surgery is technically challenging and requires sometimes a multidisciplinary approach with a thoracic surgeon.
Choose your surgeon with the training and the experience to manage these complex conditions.
Dr. Moawad is a highly reputable leading expert in this domain.
 Pudendal Neuralgia is a condition that causes long term pain that radiates throughout nerve endings of regions of the body supplied by a nerve called the pudendal nerve. This nerve runs from the lower back along the pelvic floor muscle and eventually supplies the vulva, vagina, clitoris, perineum (area between the anus and genitals) and rectum in women. In men, pudendal neuralgia affects the glans penis, scrotum, perineum and rectum.
Pudendal Neuralgia is a condition that causes long term pain that radiates throughout nerve endings of regions of the body supplied by a nerve called the pudendal nerve. This nerve runs from the lower back along the pelvic floor muscle and eventually supplies the vulva, vagina, clitoris, perineum (area between the anus and genitals) and rectum in women. In men, pudendal neuralgia affects the glans penis, scrotum, perineum and rectum.
When nerves go through sudden large trauma or repetitive small trauma, they can become irritated and cause pain. The cause of pudendal neuralgia is often trauma to the nerve during childbirth or surgical procedures. The pudendal nerve could also become entrapped by surrounding muscles and tissue resulting in similar pain. Endometriosis can produce severe scarring or inflammation that might affect the pudendal nerves.
Causes
- Childbirth trauma
- Endometriosis
- Mesh placed for urinary incontinence
- Gynecological or colorectal surgery
- Cycling
- Excessive physical exercise
- Past pelvis or perineal trauma
- Straining
- Musculoskeletal problems
Neural pain is often very variable. It could feel like burning, electric shock, shooting, aching or itching.
Symptoms
- Unilateral pelvic pain usually but may present bilaterally
- Pain is worse upon extended periods of sitting
- Pain is better standing, lying flat
- Increase in urinary frequency/urgency
- Bladder and bowel irritation
- Bladder, bowel or sexual dysfunction
Diagnosis
If you are experiencing any of the above symptoms, your gynecologist will ask you a list of questions and perform a physical exam to help with the diagnosis.
There are some diagnostic tests that you may undergo, including:
- Pudendal nerve block: the nerve is anesthetized through a vaginal injection. A relief of pain is diagnostic of pudendal neuralgia.
- Imaging such as ultrasonography or MRI to visualize the nerve entrapment site
Treatment
There are several treatment options for pudendal neuralgia ranging from conservative therapy to surgery. You and your doctor will agree on the best option for you.
- Conservative treatment:
Consists of lifestyle modifications that help with avoidance of painful triggers. These include bowel and bladder management, sitting modifications, avoiding physical activities that irritate the nerve such as cycling, and adapting your sex life with the help of a professional.
- Physical therapy:
A physiotherapist can teach you how to relax and stretch your pelvic floor muscles to ease the tension around the nerve. They can also teach you to plan your bladder and bowel management strategies.
- Medications:
Pain killers, muscle relaxants and certain types of anticonvulsants that relief neuropathic pain may be used to control symptoms but might not always help.
- Pudendal nerve block:
Similar to the diagnostic nerve block, this treatment provides temporary anesthesia to the painful nerve, leading to symptom relief.
- Surgical decompression:
If your doctor determines that you are a surgical candidate, you may opt for surgical decompression which is the most effective treatment for pudendal neuralgia as it releases nerve entrapment and destroys the nerve fibers, eliminating its painful sensation. Surgery can be done via minimally invasive techniques.
At CEAPS, we always opt for minimally invasive approaches to provide the best experience for our patients with the least amount of side effects and complications. Pudendal decompression surgery is technically challenging and requires a high level of surgical expertise.
Choose your surgeon with the training and the experience to manage these technically challenging conditions in a minimally invasive fashion.
Dr. Moawad is a highly reputable leading expert in this domain.
 Bowel endometriosis is when endometrial-like nodules grow on the surface of or inside the intestines. It can present with a single or multiple nodules of different sizes. Bowel endometriosis is estimated to be found in 5-12% of patients with endometriosis, with the rectum and sigmoid, which are the most distal parts of the large intestine, being involved in 90% of the cases. In cases where the lesions grow in the rectum and vagina, we call the condition rectovaginal endometriosis.
Bowel endometriosis is when endometrial-like nodules grow on the surface of or inside the intestines. It can present with a single or multiple nodules of different sizes. Bowel endometriosis is estimated to be found in 5-12% of patients with endometriosis, with the rectum and sigmoid, which are the most distal parts of the large intestine, being involved in 90% of the cases. In cases where the lesions grow in the rectum and vagina, we call the condition rectovaginal endometriosis.
Bowel endometriosis can be asymptomatic but may also present with the following symptoms:
- Pain when passing a bowel movement
- Straining to pass a bowel movement
- Abdominal cramps and bloating
- Pain during sex
- Diarrhea or constipation
- Blood in stools
- Bowel obstruction which manifests as an inability to pass stools or flatus and could require hospital admission and surgical resection of the lesion
Diagnosis
During your visit to your gynecologist, they will perform a pelvic and abdominal exam on you and possibly get an ultrasound. When there is suspicion of bowel endometriosis, your doctor might also order an MRI to evaluate the extent of the disease or a colonoscopy to visualize lesions inside the bowels.
This work up is important to determine the treatment and the extent of surgery, if it were to be performed.
Management
Medical therapy with oral contraceptives could be attempted to control symptoms in patients with bowel endometriosis .
In patients with severe symptoms or bowel obstruction, surgery is the optimal approach. Surgery, done laparoscopically or robotically, removes all visible lesions and sometimes requires removal of a part of the wall of the bowel( discoid resection) or section of the Bowel (segmental resection) .
The technique and extent of surgery will be determined by your surgeon on an individualized basis. Ask your doctor about the best surgery for you.
At CEAPS, we always opt for minimally invasive approaches to provide the best experience for our patients with the least amount of side effects and complications. Bowel endometriosis surgery is technically challenging and requires sometimes a multidisciplinary approach with a colorectal surgeon.
Choose your surgeon with the training and the experience to manage these complex conditions.
Dr. Moawad is a highly reputable leading expert in this domain.

Ovarian remnant syndrome (ORS) is a rare condition which results from leaving behind a part of the ovary after oophorectomy, a surgical procedure that removes one or both ovaries. The
residual tissue may cause severe pelvic pain and/or absence of menopause after oophorectomy. ORS usually presents within the first 5 years post operation.
Risk factors
-
- Endometriosis is a risk factor for ORS. It is likely that due to endometriosis, ovarian tissue may become stuck to adjacent structures and missed during surgical removal leading to ORS
- Pelvic adhesions, which may limit visualization during surgery
- Bleeding during surgery
- Poor surgical technique
- Anatomic variations, such as an unusual location of the ovary
Presentation
Patients with ORS may present to the doctor most commonly with a complaint of a pelvic mass or pelvic pain. Other symptoms include:
- Continued menstruation after removal of both ovaries. The ovary produces hormones that allow the menstrual cycle to occur. When your surgeon deliberately removes the ovaries, they expect menstruation to cease. This might not happen in ORS.
- Endometriosis-like symptoms that may include painful intercourse, and urinary or bowel complaints.
Diagnosis
A history of oophorectomy is required to make a diagnosis of ORS. If suspected, a pelvic ultrasound should be performed to look for a mass.
Blood hormone levels and imaging findings can be used to clinically diagnose patients with ORS.
A definitive diagnosis necessitates surgical exploration and removal of the residual tissue.
Treatment
Symptomatic patients generally require treatment for ORS. The mainstay of treatment involves surgical removal of the remnant ovary and can be done via minimally invasive techniques. Surgery is preferred as it negates the possibility of malignant transformation of the ovarian tissue.
For patients who are not surgical candidates, hormonal therapy can be employed to suppress what is the left of the ovarian function and control symptoms.
At CEAPS, we always opt for minimally invasive approaches to provide the best experience for our patients with the least amount of side effects and complications. ORS surgery is technically challenging and requires a high level of surgical expertise.
Choose your surgeon with the training and the experience to manage these technically challenging conditions in a minimally invasive fashion.
Dr. Moawad is a highly reputable leading expert in this domain.
 An isthmocele is an indentation or discontinuation in the uterine wall that results at the location of a Cesarean section scar. Its causes aren’t completely understood but it is thought to be related to incomplete or abnormal healing of the uterine incision. This scar defect weakens and thins out the uterine wall at its location.
An isthmocele is an indentation or discontinuation in the uterine wall that results at the location of a Cesarean section scar. Its causes aren’t completely understood but it is thought to be related to incomplete or abnormal healing of the uterine incision. This scar defect weakens and thins out the uterine wall at its location.
Isthmoceles can be asymptomatic but may produce symptoms and complications such as:
- Postmenstrual spotting
- Painful periods
- Painful intercourse
- Chronic pelvic pain
- Possible infertility
- Risk of uterine rupture or placental adhesion during pregnancy
Diagnosis
A uterine isthmocele can be detected incidentally on ultrasound or purposefully looked for by the physician if a patient is symptomatic.
The most accurate way to diagnose an isthmocele is with a saline infusion sonohysterogram (SIS). During this procedure, your gynecologist will inject a small amount of sterile saline into the uterine cavity through the vagina and visualize the lining using an ultrasound.
MRI is also used for the diagnosis of isthmocele.
Treatment
There are several ways in which a uterine niche could be treated ranging from expectant management and pharmacological treatment to surgery. Surgery could be done through open, minimally invasive, hysteroscopic and vaginal approaches. Hysteroscopy and laparoscopy are the most common approaches and desire for future fertility plays an important role in choosing a treatment modality.
- Hysteroscopy: Your doctor would shave or cauterize the defect from the inside. This works best for women with abnormal bleeding, a thick wall and no desire for future pregnancy.
- Laparoscopic repair: Your gynecologist would completely remove the defect and reconstruct the wall of the uterus. This option allows for a healthy future pregnancy as it removes the frail part of the muscle.
At CEAPS, we always opt for minimally invasive approaches to provide the best experience for our patients with the least amount of side effects and complications. Isthmocele surgery is technically challenging and requires a high level of surgical expertise.
Choose your surgeon with the training and the experience to manage these technically challenging conditions in a minimally invasive fashion.
Dr. Moawad is a highly reputable leading expert in this domain.
 A C scar ectopic pregnancy (CSEP) is the rarest form of ectopic pregnancy (pregnancy outside of the uterus) in which the embryo implants over a previous C section scar. Some risk factors have been suggested to contribute to this condition, such as hysterotomy, uterine manipulation and in vitro fertilization.
A C scar ectopic pregnancy (CSEP) is the rarest form of ectopic pregnancy (pregnancy outside of the uterus) in which the embryo implants over a previous C section scar. Some risk factors have been suggested to contribute to this condition, such as hysterotomy, uterine manipulation and in vitro fertilization.
Presentation
In general, the classic triad of an ectopic pregnancy is abdominal/pelvic pain, vaginal bleeding and a painful mass. Case reports of patients with CSEP have been described. Patients usually present with history of amenorrhea (missed menstruation), lower abdominal pain, abnormal vaginal bleeding.
CSEP could also be detected incidentally on routine first-trimester pregnancy ultrasound.
Detection
After the patient learns that she’s pregnant through a positive pregnancy test, her doctor will schedule an ultrasound for her which would visualize the implantation site of the embryo.
CSEP is considered a life-threatening emergency because it increases the risk of rupture of the uterine wall.
Management
When detected early, CSEP could be treated conservatively through dilation and curettage or methotrexate. Management could sometimes require surgical removal of the pregnancy and repair of the uterine wall.
 A tubo-ovarian abscess (TOA) is an infectious mass found in the fallopian tube, ovary or near those structures. It can be due to several factors that introduce an infection but it usually develops as a complication of a condition called pelvic inflammatory disease (PID). PID is an infection of the pelvic reproductive organs that results mainly from untreated sexually transmitted infections.
A tubo-ovarian abscess (TOA) is an infectious mass found in the fallopian tube, ovary or near those structures. It can be due to several factors that introduce an infection but it usually develops as a complication of a condition called pelvic inflammatory disease (PID). PID is an infection of the pelvic reproductive organs that results mainly from untreated sexually transmitted infections.
Bacteria can travel up the vagina into the uterus reaching the tubes and ovaries to form a walled-off cyst known as a tubo-ovarian abscess. TOAs occur in around 15% of patients with PID and are usually polymicrobial, meaning several types of bacteria are isolated from the abscess.
A TOA can be life-threatening should it rupture and cause sepsis, a widespread infection in the patient’s bloodstream.
Risk factors for developing a TOA include:
- Young age
- Multiple sexual partners
- Sexually transmitted infections
- Uterine instrumentation, such as insertion of an IUD with an active infection, or a dilation and curettage (D&C)
- Hysteroscopy
Symptoms
- Lower abdominal pain
- Fever and/or chills
- Vaginal discharge
- Painful intercourse
- Nausea & vomiting
Evaluation & diagnosis
On suspicion of a tubo-ovarian abscess, your doctor will perform a transvaginal ultrasound and may be able to identify the mass. Further imaging, usually a CT scan, might be needed to better visualize the abscess.
Although not commonly used, laparoscopy is still considered the definitive diagnostic tool and it may allow for drainage and culture of the abscess as well.
Treatment
The most important first step in management of a TOA is starting antibiotics to avoid a widespread infection. Imaging-guided drainage by a radiologist could be attempted during antibiotic treatment.
While on this regimen, patients should be monitored for worsening symptoms or lack of improvement, which would then require surgical intervention to remove the abscess along with the affected tube or ovary.
Complications
- Recurrent PIDs
- Chronic pelvic pain
- Ectopic pregnancy, outside of the uterus
- Infertility
At CEAPS, we always opt for minimally invasive approaches to provide the best experience for our patients with the least amount of side effects and complications. TOA surgery is technically challenging and requires a high level of surgical expertise.
Choose your surgeon with the training and the experience to manage these technically challenging conditions in a minimally invasive fashion.
Dr. Moawad is a highly reputable leading expert in this domain.
Call us or request an appointment with Dr. Gaby Moawad to address your condition.